What is HCC (Hierarchal Risk Adjustment)
History is ripe with examples of insurance companies denying or inflating coverage for ill patients. The Affordable Care Act (ACA) was created on the premise of extending affordable healthcare to all patients. A better framework was needed to adjust more healthcare spending towards more sicker patients and prospectively create a financial prediction for spending for future years.
The already in use Centers for Medicare and Medicaid Services’ (CMS) Hierarchical Condition Category (HCC) risk adjustment model (it uses health status in a “base year” to predict costs in the following year) gained significance at this time. The prospective risk adjustment model is used to calculate risk scores so as to adjust capitated payments made for aged and disabled beneficiaries.
“Hierarchical condition category coding helps communicate patient complexity and paint a picture of the whole patient
~ American Academy of Family Physicians”
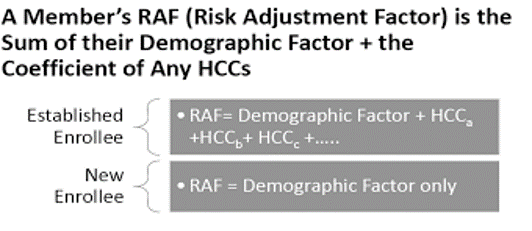
HCC is one of the many judicious ways to code the risk-adjustment of patients. It is based on the International Classification of Diseases -10 (ICD-10) coding scheme, where risk scores are assigned to each patient by considering their recent medical condition. The ICD-10 codes along with patient demographics (i.e. gender and age) are mapped with HCC coding to determine the actual Risk Adjustment Factor (RAF) score. The insurance companies then predict patients costs by analyzing their RAF scores. The RAF Score is then used as a multiplier to budget and direct more spending flow towards patients who need it more.
According to the American Academy of Family Physicians, “hierarchical condition category coding helps communicate patient complexity and paint a picture of the whole patient”. Hence it is useful to precisely measure cost, performance, and quality.
What is HCC Review?
Risk Adjustment is the mechanism used by various governments and payers to adjust the revenue based on the diverse health status of the covered population. There are many benefits of HCC Risk Adjustment namely, allocation of sufficient funding, aligning incentives with the rewards (the triple aim outcomes), optimizing quality and efficiency.
HCC Review is the process of capturing insights from the available voluminous data to find coding gaps or coding errors that lead to an inaccurate assessment of the patient’s clinical profile. Before the HCC Coding and risk adjustment process, the population looks like this.
After accurate HCC coding, the population now looks like this painting a more complex picture of the population segments.

HCC Review can be termed as the process of ensuring that the complexity of patient segments in terms of clinical conditions is being as accurately documented as practically possible. The first part of the HCC review is to aggregate and collate data from multiple sources i.e. Medical Record Review, RX Claims, Hospital claims, provider claims, in-home assessments and other supplemental data files such as ADT (Admission, Discharge and Transfer. Usually, this data is available with the EMR and an aggregation is not required.
To enable the State and Federal government to appropriately allocate revenue to the high-risk members enrolled, patient coded date (medical information submitted on physician claims for each patient) is essential requirement. Specificity of diagnosis coding is substantiated by the medical record. Accurate coding helps to best reflect the cost of caring for members/patients: It demonstrates the level of complexity for the patient encounters. ü It is vital to a healthy revenue cycle, and more important, to a healthy patient. There are some cardinal rules of coding patient data which create a baseline check for our initial HCC review:
- Existing Conditions are Documented – A review checks whether the condition is coded accurately, or the coded condition actually exists.
- Diagnoses are episodic and do not roll over from one visit to another – A patient who has a missing limb need to be recoded again in the next year else the system will think that the patient grew a limb.
- Same condition can be coded multiple times for relevance, accuracy and recency.
- Co-existing conditions provide a holistic view of the patients and much be coded together.
It is the duty of the coders to review medical records to stratify and identify patients with HCC conditions where there is an improved opportunity for accurate reflection of the patient conditions. The review can be done prospectively, retrospectively or concurrently.
Types of HCC Review
There are three types of HCC review processes Prospective, Retrospective and Concurrent review.
- Prospective Review – A prospective review assists provider prepare for scheduled/upcoming patient encounters.
- Concurrent Review – It is similar to real time review but has some lag where HCC coders examine the patient chart, clinical notes and HCC codes prior submitting claims to payors. Concurrent review may be enabled in real time by emerging technology such as Wiseman 360Platform.
- Retrospective Review – This type of review is done usually weeks or months after patient encounter and claims submission process has been completed. The aim is to carry out a post-audit and potentially uncover unreported HCC codes and wrongly reported HCC codes.
It is a good idea to combine prospective and concurrent review to ensure accurate documentation and claims. As a good practice, prospective review is an upstream activity that can enable providers to take maximum advantage of the upcoming patient encounter and the “right at the first” accuracy of their prospective claims. Prospective reviews increase the potential for improved and accurate documentation to avoid duplicate work or others. A higher weightage should be given to prospective reviews which can be combined with concurrent reviews to capture any breadcrumbs that may cause errors.
Another use case for HCC review is where technology enablers allow providers to asses the impact of patients who have not visited the providers for long periods. Although challenging to achieve this manually, new technologies have allowed us to prompt providers to call these patients for a visit, improving clinical outcomes as well as financial performance of a practice.
Why is HCC coding important for practitioners and ACOs
It should be clear that HCC coding is a great equalizer for the practitioners and ACOs. Before the widespread adoption of HCC risk adjustment model, the reimbursements used to be made entirely on the basis of patients’ demographics. It was well established that patient healthcare costs vary on case to case basis, and therefore the payers rightly had certain concerns over irrational payments. Before HCC model, there was no formalized way to encode and decode those differences in population health segments, hence the payers and CMS reverted to the prevalent default way of generic allocation of funds to patients irrespective of their conditions.

The funding allocated for patients with HCC conditions in the current year can be adjusted (moved up or down) based on the changing clinical profile of the patient for the prospective year. Using the illustration above, if the weighing scale on the HCC risk adjusted weight side is more than the benchmarked budgeted cost, CMS would allocate more funds next year for this patient to equalize the scale. Inversely, if the weighing scale on the HCC risk adjusted side weights less than the benchmarked budgeted cost, CMS would allocate less funds next year for this patient. It is easy to see that HCC coding illuminates the path forward for regulators and payers who want to improve patient care while allocating appropriate funds where they are needed.
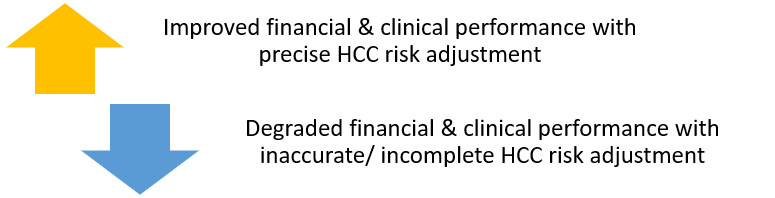
The HCC coding model helps in precision weighting the patients’ clinical problems thereby improving the accuracy of the payment system. Practitioners can significantly improve care outcomes by accurately coding patient’s clinical conditions enabling the accurate determination of RAF Scores. In turn, the accurate coding and RAF Scores help the government and payers direct funding where it will have maximum impact.
Accurate RAF score enables the clinicians to have current and relevant information of the patients’ clinical conditions, based on which diagnoses and treatments can be delivered creating high impact on the healthcare ecosystem. Precise RAF scoring of the patients also yields benefits for the coders and providers in improving revenue cycle management. Conversely, the incomplete or inaccurate RAF scoring may result in losses and reduced prospective budget allocations from the CMS. In summary, accurate coding has a positive cascading ripple effect in the system where everyone wins.
Types of HCC Coding Frameworks
The HCC model was designed by Centers for Medicare & Medicaid Services (CMS) in 2004, to estimate the potential healthcare cost a patient may bear in future and leads to ensuring the value-based payment methodologies for them. There are different risk scoring models that are currently being used in the United States. However, in this post, we will only be focusing on the following two widely used categories:
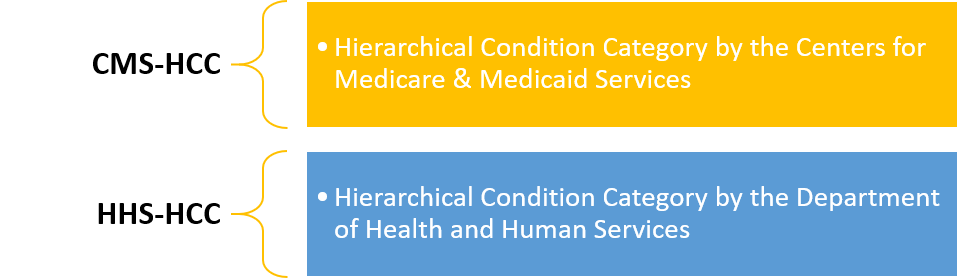
CMS-HCC
- As obvious from the name, it is a CMS based HCC model that is used for the risk adjustment of the Medicare Advantage program.
- It is aimed for the patients with over 65 age, and addresses the disabled patients.
- CMS-HCC is basically a prospective model that requires patients’ diagnosis of a base year to foresee their healthcare costs for the upcoming year.
- The patients’ data is captured by using regular Medicare processes.
- The risk adjust for these patients includes the parameters like their demographics, health conditions and institutional status.
HHS-HCC
- As obvious from the name, it is an HHS based HCC model that is used for the risk adjustment of the commercial payer populations.
- It is intended for the patients of all ages.
- HHS-HCC is basically a concurrent model that requires patients’ diagnosis of the current benefit year to determine their medical and drug expenditures of the same year.
- The risk adjust for these patients includes the parameters like their demographics, health conditions and financial status.
HCC Categories
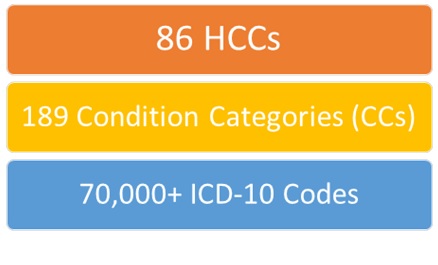
There are around 70,000+ ICD10 Codes that are grouped among 189 HCC Categories and every year around 75-85 HCC categories are picked by the CMS to drive their Medicare and MA risk adjustment models. For instance, in the latest available CMS-HCC Model Category V24, we have 86 HCC Categories with around 9700 ICDs.
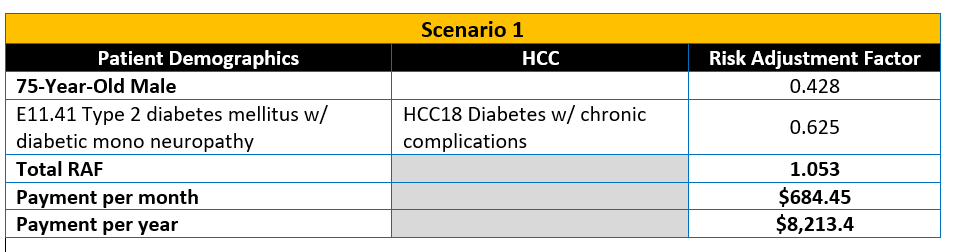
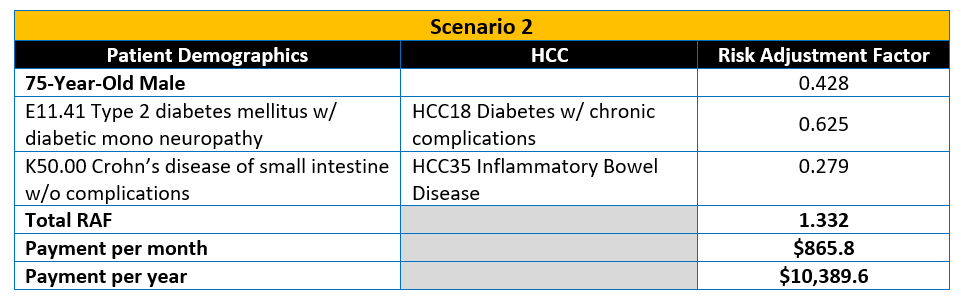
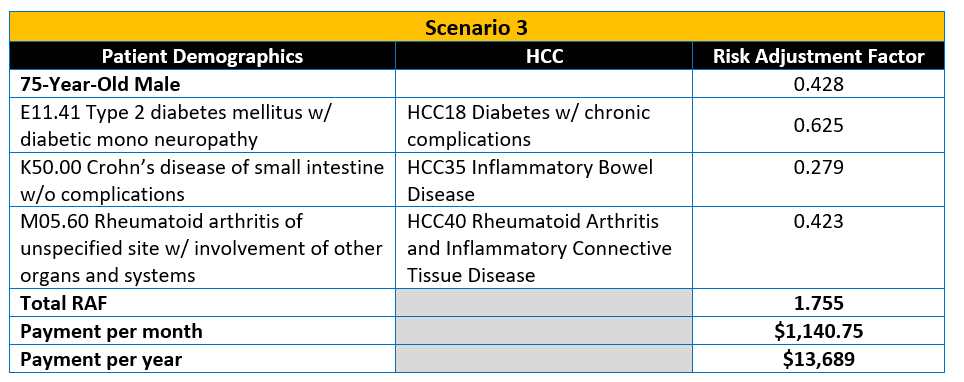
We will discuss a sample use case that shows how HCC coding could affect the capping of a 75 year old male patient’s benchmark.
HCC Coding – Use case
Let us assume that the capitated rate of a CMS plan is $650 per member per month (PMPM) that should be adjusted on the basis of HCC scores. In scenario 1, there are coding gaps create an inaccurate medical profile of the patient.
CMS and payers are increasing placing more emphasis on accurate documentation of HCC scores and organizations that are not ready for the changing ecosystem are either leaving money on the table or run serious compliance risks due to over-documentation without supporting evidence. As providers are not coders, accurate coding remains a major challenge which is being solved using technology enablers. These enablers improve claims accuracy, coder productivity, recapture rate and HCC benchmarking. Emerging innovative technologies are making it possible to communicate in near real time to providers to fix costly coding mistakes during and within the patient encounter time. The end result is improved productivity and HCC recapture rate.
References
- The Centers for Medicare & Medicaid Services (CMS)
https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Risk-Adjustors - The Centers for Medicare & Medicaid Services (CMS). 2008 Risk Adjustment Data Technical Assistance For Medicare Advantage Organizations Participant Guide.
https://www.csscoperations.com/Internet/Cssc3.Nsf/files/participant-guide-publish_052909.pdf/$File/participant-guide-publish_052909.pdf - The American Academy of Family Physicians (AAFP)
https://www.aafp.org/practice-management/payment/coding/hcc.html
